Specific gut bacteria may be associated with pulmonary arterial hypertension - Science Daily
Specific gut bacteria may be associated with pulmonary arterial hypertension - Science Daily |
- Specific gut bacteria may be associated with pulmonary arterial hypertension - Science Daily
- Daring to Be Rare by Believing in the Power of Hope - Pulmonary Hypertension News
- Positive data send United Therapeutics' shares surging - The Pharma Letter
| Specific gut bacteria may be associated with pulmonary arterial hypertension - Science Daily Posted: 24 Feb 2020 04:54 AM PST Researchers have identified a distinct collection of bacteria found in the gut that may contribute to and predict the development of pulmonary arterial hypertension (PAH), according to new research published today in the American Heart Association's journal Hypertension. PAH is a chronic and progressive disease in which the arteries that supply blood to the lungs are constricted, resulting in symptoms such as shortness of breath, heart palpitations, fatigue and others. In PAH, persistently high blood pressure in lung arteries makes the right side of the heart work too hard to pump blood, resulting in right-sided heart failure (inability of the heart to pump blood adequately). It is much less common than systemic blood pressure, which represents the force of blood moving through blood vessels throughout the entire body. Everyone has a collection of bacteria in their gut -- known as microbiota -- that aid in digestion. The researchers found that having a specific microbiota profile in their gut predicted the presence of PAH with 83% accuracy. "We showed for the first time that specific bacteria in the gut are present in people with PAH. While current PAH treatments focus on the lungs, looking at the lung/gut axis could open the door to new therapies centered in the digestive system," said Mohan Raizada, Ph.D., lead study author and distinguished professor in the department of physiology and functional genomics at the University of Florida College of Medicine in Gainesville, Fla. For the study, stool samples were collected from 18 PAH patients and 12 people without a history of cardiopulmonary disease. The microbiota DNA from the stool samples were isolated and sequenced. The testing revealed a group of bacteria unique in the PAH patients that were associated with PAH. This is the first link between a specific collection of bacteria and pulmonary arterial hypertension. However, it is not the first time that gut bacteria have been connected to medical conditions. A variety of different gut microbiota profiles have been linked to a variety of cardiovascular diseases including high blood pressure. "We were very surprised to see such an association within a small group of study subjects," said Raizada. "It usually requires hundreds of patients to achieve such significance." Gut microbiota are constantly changing, depending on what we eat, our environment and especially our genetic makeup. However, Raizada said the bacteria associated with PAH are unique and do not seem to change: "We believe these particular bacteria are constant." If the results are validated in a larger study, the researchers said that the unique bacterial profile could help to diagnose PAH early, possibly replacing the invasive heart catheterization that is used today to diagnose the disease. Also, new types of treatment focused on altering the gut microbiome of PAH patients could be developed, providing new hope for halting the progression of the disease. Another important question to be researched is how the gut bacteria impacts the lungs of PAH patients. "We do not know if and how gut bacteria and viruses make their way to the lungs," said Raizada. "Some studies have pointed to an increased incidence in intestinal leakage among people with pulmonary hypertension, which may allow some intestinal bacteria to get into the bloodstream and circulate to the lungs where they can cause inflammation and lead to vascular changes." "There is still the question of whether the specific microbiota associated with PAH is the cause or the result of the disease, therefore, more research is needed," concluded Raizada. Co-authors are: Seungbum Kim, Ph.D.; Katya Rigatto, Ph.D.; Marcelo Gazzana, M.D.-Ph.D.; Marli Knorst, M.D., Ph.D.; Elaine Richards, Ph.D.; Carl Pepine, M.D. Author disclosures are in the manuscript. The study was funded by grants from the National Institutes of Health (NIH), the NIH National Center for Research Resources and the U.S. Department of Defense. |
| Daring to Be Rare by Believing in the Power of Hope - Pulmonary Hypertension News Posted: 24 Feb 2020 07:00 AM PST Year-round, the parent company of this website, BioNews Services, strives to provide pertinent and updated information about complex, rare diseases. Staying current with medical research is a key component of effective self-advocacy, but personal experience is also a gold mine of valuable information and inspiration. BioNews recognizes this by encouraging conversation within the forums of each rare disease website. The company also inspires patients and caregivers to spread awareness by sharing personal struggles and triumphs beyond their specific communities. Doing so creates camaraderie among all those suffering from a rare illness. It also educates and stimulates compassion from those who are fortunate to have no clue of what being sick with a rare disease is like. Most importantly, sharing personal stories might be the "aha!" moment that leads someone to an earlier diagnosis. In recognition of Rare Disease Day on Feb. 29, BioNews has started a campaign. Those living with a rare disease are encouraged to storm the internet with personal stories, pictures, and videos. We are being asked to include the hashtag #WhatMakesMeRare ending in the initials of our rare disease, for example, #WhatMakesMeRarePH. Pulmonary hypertension is a very rare, incurable, and life-threatening condition that affects the arteries in the lungs and the right side of the heart. Treatments can provide a better quality of life for an uncertain amount of time, but when they stop helping, hope begins to fade. Not everyone is eligible for the second chance at life that a lung transplant, or even rarer, a heart and double-lung transplant, can provide. Therefore, my son Cullen is extremely rare. He was diagnosed with idiopathic pulmonary hypertension at 8 years old and received a heart and double-lung transplant when he was 14. In August 2019, he beat the discouraging odds of survival by celebrating five years post-transplant. Despite difficult and ongoing challenges, he continues to thrive. But as his mom and caregiver, what makes me rare? Mothers often check on their sleeping child, but when I did, it was to make sure Cullen was still breathing. I spent many sleepless nights watching him struggle. Weekday mornings were especially heartbreaking because I had to assess whether Cullen was well enough to attend school. Labored breathing and chest pains often kept him home. My husband and I were accustomed to making quick decisions about who would stay home from work, how our other son would get to school, and what our game plan would be if Cullen needed to see a doctor, visit the emergency room, or be admitted to the hospital. For this reason, I always had a bag packed and stored in our car for unexpected emergencies. After he was listed for transplant, we lived out of suitcases for a year so that we could move quickly when Cullen received the call. Children notoriously ask difficult questions, but I don't think it's common for little ones to inquire about their own mortality. Cullen was in fourth grade when he started expressing concern that he was going to die young. I had never heard of PH before his diagnosis. Trying to console my child with hope regarding a disease that at the time I knew little about was beyond difficult. 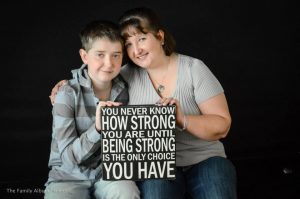 I've seen my son through more tests, treatments, and surgeries than rites of passage. Having advocated for Cullen for more than a decade, I've become well-versed in medical jargon. Research and honing my listening skills helped me to become very knowledgeable about my son's health concerns. Sometimes I'm asked if I'm a nurse or a doctor. This honorary medical degree I seemed to have earned is something I know I share with most parents of ill children. Cullen was born healthy and didn't become symptomatic until he was 6. For a long time, my family grieved the normalcy that we once enjoyed. Memories were reminders that when Cullen became rare, we all did, too — mother, father, and brother. The loneliest leg of the journey was the two years he went misdiagnosed. The agonizing battle to reach a correct diagnosis is a common one that those living with rare diseases often fight. It's also the reason why so many of us make a huge effort to share our experiences. We might not have the knowledge to find a cure, but we can at least help others recognize symptoms so they can benefit from an early diagnosis. What makes me inconsolably rare is that I'm 48, and unlike most women my age, I have known more children who have died than adults. Therefore, I find it equally important to share Cullen's life since transplant. There was a time when stories like this provided hope to us, and now it's our turn to pass hope on to others. Dare to be rare by believing in the power of hope when others might not. *** Note: Pulmonary Hypertension News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Hypertension News or its parent company, BioNews Services, and are intended to spark discussion about issues pertaining to pulmonary hypertension. |
| Positive data send United Therapeutics' shares surging - The Pharma Letter Posted: 24 Feb 2020 09:31 AM PST A positive result from the INCREASE study sent shares in the USA-based lung specialist United Therapeutics (Nasdaq: UTHR) soaring nearly 8% in morning trading on Monday. The study, which is testing Tyvaso (treprostinil) in people with pulmonary hypertension associated with interstitial lung disease (PH-ILD), met its primary efficacy endpoint, improvement in six-minute walk distance (6MWD). Tyvaso increased six-minute walk distance by 21 meters, compared with placebo. Significant improvements were also observed in each of the study's secondary endpoints. Chief executive Martine Rothblatt said: "I am pleased to announce the successful outcome of the INCREASE Phase III trial of Tyvaso in a unique kind of pulmonary hypertension, a variant that has no approved therapy." She added: "Some 30,000 Americans suffer from this disease, called WHO Group 3 Pulmonary Hypertension." United said it would submit the results to the US regulator by mid-year in support of an efficacy supplement to the therapy's label. For the first three quarters of 2019, United posted revenues of $402 million, down from $413 million for the comparable period of 2018. Revenues from Tyvaso represent around a quarter of that amount. In the market for pulmonary arterial hypertension treatments, United competes with GlaxoSmithKline (LSE: GSK), with its Flolan (epoprostenol), as well as Johnson & Johnson (NYSE: JNJ), with Veletri (epoprostenol) and Uptravi (selexipag), and Pfizer (NYSE: PFE), with Revatio (sildenafil). United also sells Remodulin (treprostinil) in this therapy area. |
| You are subscribed to email updates from "pulmonary hypertension diagnosis" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment