Eurordis Urges Expansion of Newborn Screening Initiatives Across... - Pulmonary Hypertension News
Eurordis Urges Expansion of Newborn Screening Initiatives Across... - Pulmonary Hypertension News |
- Eurordis Urges Expansion of Newborn Screening Initiatives Across... - Pulmonary Hypertension News
- Considering Therapy Based on PH and PAH Subpopulations - AJMC.com Managed Markets Network
- Nicotine Inhaled Often, as with E-cigarette Use, Linked to PH in Mice - Pulmonary Hypertension News
| Eurordis Urges Expansion of Newborn Screening Initiatives Across... - Pulmonary Hypertension News Posted: 25 May 2020 05:00 AM PDT European authorities must step up efforts to screen babies for a multitude of genetic disorders, a panel of experts suggested during a May 14-15 online medical conference. The session was part of the 10th European Conference on Rare Diseases & Orphan Products (ECRD2020) — which was to have occurred in Stockholm, but instead took place online via Zoom.  "We're interested in this topic because our community feels poorly served by newborn screening," said Nick Meade, policy director at Genetic Alliance UK, a national charity representing more than 230 British patient advocacy organizations. Meade said a newborn screening "patient charter" — launched in July 2019 — has already been endorsed by some 50 rare disease groups in Great Britain. "We care because a child born with a treatable rare condition with an immediate onset can be identified quickly; appropriate care, support and treatment can begin as soon as necessary to minimize the impact of the condition," Meade said. "Treatments that stop the progression of a condition can be delivered before any impact can occur." Timely treatment can result in the quick delivery of medicine, diet or some other intervention that might mitigate some conditions completely. In addition, timely information may help prospective parents avoid a "diagnostic odyssey" and give them the option of making reproductive choices. "Screening at birth can provide information to parents of a child with a rare condition much earlier than they would otherwise receive it. And the benefit of a diagnosis with rare disease is broad," Meade said. "The avoidance of an agonizing and frustrating diagnostic odyssey that might take years — and that might deliver some incorrect diagnoses along the way — is an advantage to screening in itself." Screening programs vary widely across EUECRD2020 attracted some 1,500 delegates from 57 countries and was the first all-virtual conference ever hosted by Eurordis, a Paris-based coalition of national rare disease associations. Eurordis and its co-organizer, Orphanet, used the occasion to appeal to the European Union in Brussels to urgently approve standardized policies to advance the health and well-being of all Europeans. According to the International Society for Neonatal Screening, the number of conditions for which babies are screened, as of 2018, varied from only one or two in Belarus, Croatia, Latvia, Moldova, Poland, Romania, Slovenia and Ukraine, to 20 or more in Austria, Hungary, Iceland, North Macedonia, Portugal, Spain, Slovakia and Sweden. Sadly, Britain does not score highly when it comes to newborn screening, Meade said.  "Research for some conditions requires newborn screening for case identification," he said. "There are clinical trials currently recruiting overseas that would be impossible to deliver in the U.K. because we don't have the screening programs. "Also, also new medicines receiving regulatory approval at the moment require early or pre-symptomatic administration, which is impossible without screening," he added. Having a newborn baby screened for an array of potentially damaging genetic conditions also gives parents the opportunity for reproductive choice and planning, Meade said. "It allows couples to exercise reproductive choices if they want to, and the timing of the learning of this information can be crucial, because without screening, parents might only find out in their child's third or fourth year of their risk, which means they might miss the opportunity for reproductive choices," Meade said. PKU was first disorder to be screenedOn the flip side, he said, there are some limitations to newborn screening. These include parental anxiety due to false positives for the short period between the announcement of further investigations and the all-clear, as well as indeterminate results – those who might need monitoring and further surveillance without conclusive diagnosis. In addition, there's a risk of over-diagnosis and over-treatment, particularly of conditions with a spectrum including mild forms, as well as stigmatization — the idea that the label of having a condition might be worse than the early diagnosis to a family or an individual. 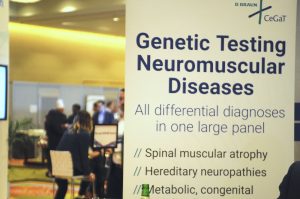 Furthermore, children cannot consent to the process, which becomes more of an issue with later-onset conditions such as Huntington's disease and declaration of carrier status. "Without minimizing the importance of these limitations, the majority of people living with serious rare conditions don't weigh these issues highly," Meade said. "That's largely because they've experienced their lives with very little access to information about diagnosis." Neonatal screening started in the 1960s and 1970s after phenylketonuria (PKU) turned out to be a treatable condition. PKU is an enzyme deficiency that can impair brain development; it occurs in 1 in 18,000 newborns and the treatment is a diet low in phenylalanine. In that test, a baby's heel was pricked, blood was placed on a "Guthrie card" that was mailed to a lab, which tested the blood for the presence of the disease. "But when this happened, people felt this was such a big possibility – that all children diagnosed with PKU should be put on a special diet as soon as possible," said Martina Cornel, professor of community genetics and public health genomics at the Amsterdam University Medical Centre. "Even if it was a rare condition, it was an important health problem." The potential of genome sequencingThese days, a modern tandem mass spectrometry newborn screening test — introduced in the 1990s — allows for the detection of up to 50 conditions including PKU. And genome sequencing in the newborn could detect at least 884 conditions, said Meade. Meade said the potential of genome sequencing in the newborn should be examined in a pilot program — though it remains to be seen whether such a program is cost-effective, which conditions should be screened for, and how those conditions should be selected. "Families affected by conditions that are not screed for at birth face a diagnostic odyssey — thankfully now significantly shortened — plus the missed opportunities for treatment, information, planning and progress in understanding the condition that could have come from a screening program." In 2010, only a handful of countries screened for 20 conditions or more: Austria, Hungary, Iceland, Netherlands, Portugal, and Spain, said Cornel, who's also vice-chair of the Dutch Patient Alliance for Rare and Genetic Diseases (known by its Dutch acronym VSOP). "In the Netherlands, we started screening for PKU in 1974, and in 2006 we added many more diseases. We now screen for more than 20," she said, noting that some European countries such as Albania still don't offer newborn screening at all. "All newborns need to be offered screening programs," Cornel said. "The goal is to identify infants with conditions for which effective therapy is available. Early treatment can prevent or ameliorate the disease, so that affected children can live healthier lives." Other speakers at the newborn screening panel included Richard Scott, MD, clinical lead for rare diseases at Genomics England, Sara Hunt, CEO of Alex, a leukodystrophy charity, and Simona Bellagambi of UNIAMO, the Italian Federation for Rare Diseases. |
| Considering Therapy Based on PH and PAH Subpopulations - AJMC.com Managed Markets Network Posted: 05 May 2020 12:00 AM PDT Elucidation of the various treatment strategies used in PH and PAH subpopulations: CTEPH, CTD-PAH, and POPH. Elucidation of the various treatment strategies used in PH and PAH subpopulations: CTEPH, CTD-PAH, and POPH. Transcript In general, we want to treat those patients as aggressively as possible because of that risk. We know that if we are not as aggressive as we should be, the patients struggle more than perhaps some of the other subgroups. It's also very interesting that some of the information has shown that using 2 oral medications in different pathways as soon after diagnosis as possible—what's called upfront combination oral therapy, which was shown in the AMBITION trial to be beneficial to Group 1 PAH patients—also holds value in connective tissue disease. Based on that scientific information and personal experience, I advocate for patients with connective tissue disease–associated mild or intermediate PAH to start 2 oral drugs as early as possible after diagnosis. Obviously, if they're sicker, they may have to be on an infusion therapy or triplet therapy. For patients with liver disease and portopulmonary hypertension [POPH], the goal is not only to treat the pulmonary hypertension [PH] but also to allow the patient to safely receive a liver transplant. Ultimately, the problem is end-stage liver disease or hepatic cirrhosis. If that's not remedied, even if you control and improve the pulmonary hypertension, patients are still at risk of having complications from cirrhosis or even dying from liver failure. The goal is to get pressures down to a certain level, typically a mean pulmonary artery pressure of 35 mm Hg or less, with low pulmonary vascular resistance and normal right ventricular function by echocardiography, which then allows the patients to safely receive a liver transplant. We work carefully with our GI [gastrointestinal] hepatologists and our liver transplant surgeons. We discuss these patients carefully at multidisciplinary conferences regarding the best therapy and the goals of therapy that can get them in an appropriate condition such that they can undergo a liver transplant if they're otherwise eligible, which has a very good chance of improving the pulmonary hypertension as well. It's not a guarantee that pulmonary hypertension would go away completely, but there is often a very favorable response, at least allowing for less medication after the transplant. Certainly, patients feel better if their liver is now working properly. For Group 4 chronic thromboembolic pulmonary hypertension [CTEPH], decisions around drug therapy really hinge on if the patient is eligible for surgery—pulmonary thromboendarterectomy—which if successful, has a very high cure rate. About 10% of patients may have persistent pulmonary hypertension after the surgery, so they may require ongoing medication. Almost always, the initial therapy in that group, if they're not going to have surgery, is riociguat. A new intervention that's receiving more study is balloon pulmonary angioplasty. There is some information showing that it can have a very positive effect on pulmonary pressures and pulmonary vascular resistance with similar or even slightly better benefit than riociguat, based on 1 study. But remember, it's an intervention, so it's going to have complications. Complications can be severe when you're working with a catheter in pulmonary circulation. The potential complications may balance out any potential improvement over drug therapy. That becomes an individualized decision between the physician and the patient. But we're very excited about the possible role of balloon pulmonary angioplasty in these patients who would not otherwise be eligible for the more curative surgery, pulmonary thromboendarterectomy. |
| Nicotine Inhaled Often, as with E-cigarette Use, Linked to PH in Mice - Pulmonary Hypertension News Posted: 22 May 2020 08:00 AM PDT Chronic inhalation of nicotine, the addictive component of all tobacco products, is enough to trigger changes in pulmonary arteries and in the heart's right chamber that can cause pulmonary hypertension (PH), a recent study in mice found. The study, "Effects of Chronic Nicotine Inhalation on Systemic and Pulmonary Blood Pressure and Right Ventricular Remodeling in Mice," was published in the journal Hypertension. Pulmonary hypertension is a chronic and progressive disease in which the pulmonary arteries become narrowed and blocked, requiring the heart to pump harder for blood to flow through these blood vessels. This extra effort can enlarge and weaken the heart, and lead to heart failure. Cigarette smoking is known to be associated with pulmonary hypertension in people and in animal models, but the role of nicotine in the disease is less well understood. In the era of electronic cigarettes (e-cigs), which allow nicotine to be inhaled as a vapor and are rising in use as cigarette smoking declines, determining if a link exists between this compound and disease is important. Researchers at Louisiana State University Health Sciences Center investigated how chronic nicotine inhalation affected blood pressure, pulmonary artery pressure, and cardiac function in mice exposed to normal or nicotine-filled air for 12 hours each day for eight weeks. "The murine [mouse] nicotine inhalation model employed in this study closely mimics human smokers/e-cig users, in terms of route of nicotine exposure, dosage, and chronicity (over 8-week period in mice)," the researchers wrote. They found that nicotine-exposed mice exhibited high systolic blood pressure — the pressure in arteries during the contraction of the heart — as early as the first week of exposure. This increase lasted through week three then returned to normal levels over weeks four through eight, suggesting a development of tolerance to nicotine or compensatory mechanisms coming in to regulate blood pressure. "The increase was transient, but was sufficiently long to pose potential health risks in individuals with preexisting cardiopulmonary conditions," Eric Lazartigues, PhD, professor at LSU Health New Orleans School of Medicine, said in a press release. At the end of the eight weeks, nicotine exposure had led to pulmonary hypertension, with exposed animals showing higher blood pressure in their right ventricle — which pumps blood into the lungs — along with a thickening of the walls and right ventricle enlargement. The left ventricle — responsible for pumping blood to the rest of the body — was not affected. "Interestingly, the adverse effects of inhaled nicotine are largely isolated to the right heart, as we found no significant changes in left heart remodeling or protein expression," said Xinping Yue, MD, PhD, a professor at LSU School of Medicine. The team believes that these changes in the right ventricle of nicotine-exposed animals were likely caused by the excess production of the ACE protein and activation of the MAPK signaling pathway — both associated with pulmonary hypertension. Pulmonary vessel remodeling, a disease hallmark, was also observed in nicotine-exposed animals. But while nicotine did not increase artery wall thickness, it did cause some arterioles that normally not covered by muscle cells to become muscularized. "Our study, for the first time, shows that chronic inhalation exposure to nicotine alone in mice leads to PH with pulmonary vascular and [right ventricular] remodeling," the researchers wrote. "This study should help raise the awareness of the adverse effects of nicotine inhalation on the cardiopulmonary system and help formulate public health policies on e-cigarettes," said Jason Gardner, PhD, also a professor at the LSU School of Medicine. |
| You are subscribed to email updates from "pulmonary hypertension symptoms" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment